Enhancing the Anti-tumor T Cell Repertoire
Why Most Endogenous Anti-Tumor T Cells Are Not So Good
Although many mechanisms that cancer or immune cells use to inhibit anti-tumor immune responses can be therapeutically antagonized, a major bottleneck that stymies the ability of T cells to eradicate cancer lies within the T cell repertoire. T cells rely on their T cell receptor (TCR) to recognize and attack cancer cells through the binding of the TCR to cancer-associated antigens. There are two main types of cancer-associated antigens: 1) neoantigens that arise from mutated proteins, and 2) tumor self-antigens that are found on normal tissue but aberrantly expressed by the tumor. The strength of this TCR-antigen interaction is important. Unfortunately, high affinity neoantigens are often eliminated during tumorigenesis due to cancer immunoediting, and TCRs against tumor self-antigens are often weak due to a process called central tolerance. Here, T cells that possess high affinity TCRs against potential tumor self-antigens are deleted during T cell development in the thymus — a normal process that prevents accumulation of strong auto-reactive T cells that can cause autoimmunity. Thus, a typical tumor-reactive T cell repertoire is largely devoid of T cells that strongly recognize tumor antigens.
The tumor-reactive T cell repertoire is limited by immunoediting and central tolerance. T cells with strong TCRs against neoantigens and tumor self-antigens are often scarce. How does this impact the propensity of tumor-infiltrating T cells to become exhausted vs. effector-memory (bottom)?
Temporarily Interrupting T Cell Development Releases Tumor-Directed T Cells with Auto-Reactive Features
Central tolerance relies on specialized cells in the thymus to present self-antigens to developing T cells and delete those that strongly recognize these self-antigens. This process is critical in preventing autoimmunity, and its importance is thought to make the T cell repertoire essentially immutable. However, our collaborator, Dr. Mark Anderson, discovered that a blocking antibody against RANKL (anti-RANKL) can temporarily interfere with central tolerance, resulting in the transient egress of potentially auto-reactive T cells that normally would have been deleted in the thymus. What happens if anti-RANKL is used for cancer immunotherapy? Does the T cell repertoire now contain auto-reactive T cells that can strongly recognize tumor self-antigens? Using mice bearing a poorly immunogenic melanoma tumor, we discovered that anti-RANKL does indeed alter the peripheral T cell repertoire generated after immune checkpoint blockade (ICB). When examining CD8 T cells against a melanoma tumor self-antigen called TRP2, we find subpopulations that possess TCRs with auto-reactive features and high affinity against TRP2.
Interrupting central tolerance with anti-RANKL alters the T cell repertoire against the TRP2 tumor self-antigen after ICB. TCRs possess auto-reactive features within amino acids that contact peptide/MHC and show higher affinity against TRP2.
High-Affinity T Cells with Auto-Reactive Features Can Circumvent T Cell Exhaustion
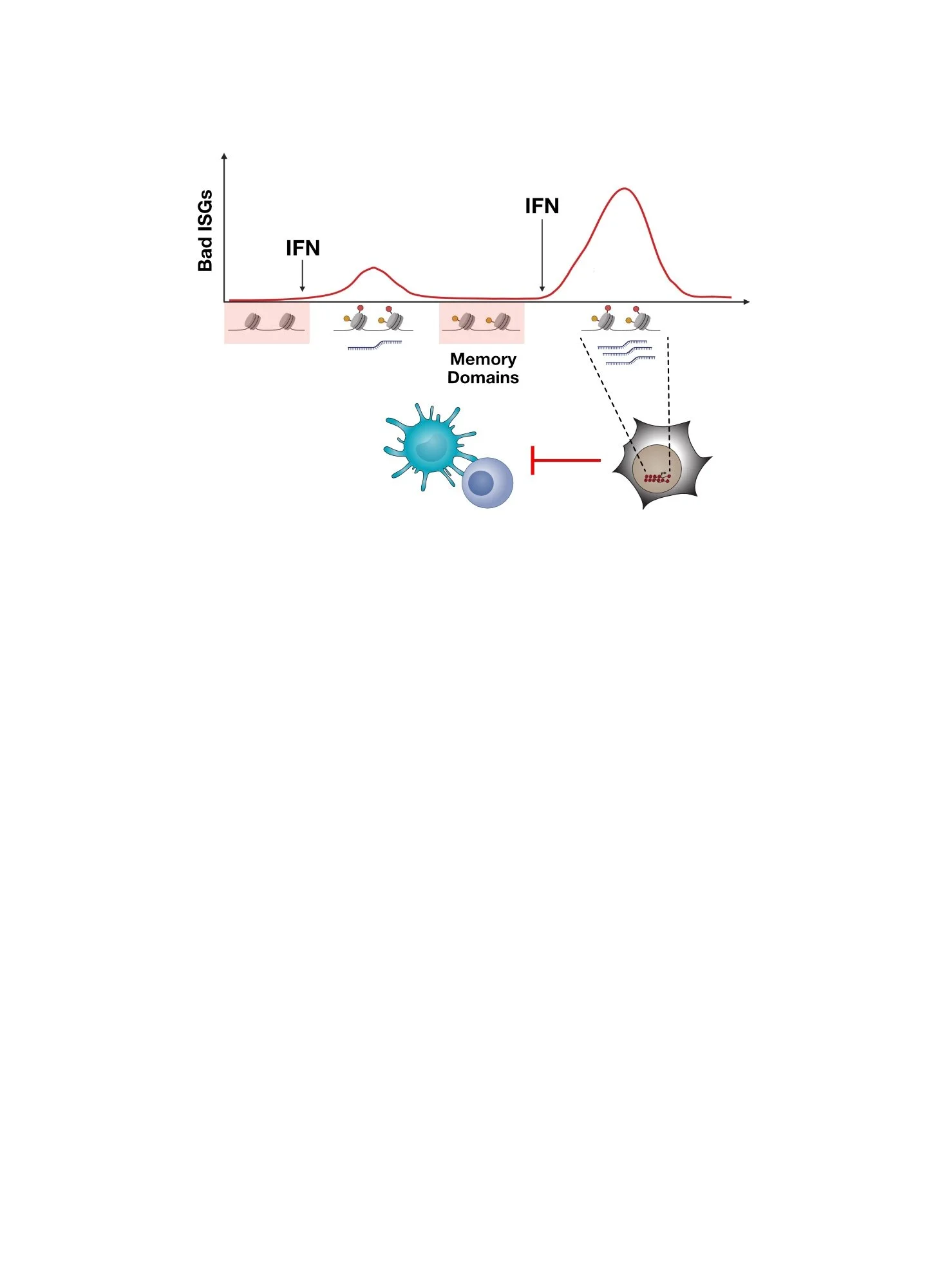
Are the auto-reactive T cells with higher-affinity TCRs against tumor self-antigen better at attacking cancer? After ICB, most CD8 T cells in a tumor are sub-optimally activated by antigens and become terminally exhausted T cells, which are T cells with poor effector function that limits the efficacy of ICB. In contrast, by tracking individual T cells using single-cell sequencing methods, we discovered that high-affinity tumor-reactive T cells generated by anti-RANKL are effectively primed in the lymph node and then traffic to the tumor where they exhibit increased TCR signaling and a transcriptional program that interferes with T cell exhaustion. Thus, rather than becoming exhausted, these T cells become memory-precursor and effector-memory T cells against tumor self-antigens.
T cell clonotype (aR.C1) generated after anti-RANKL possesses TCR with auto-reactive features. This T cell is primed in the lymph node, has enhanced TCR signaling strength, and becomes effector-memory T cells in the tumor.
Poorly Immunogenic Tumors Lacking Strong Neoantigens Are Rejected By T Cells Generated by RANKL Blockade
Having provisioned the T cell repertoire with high-affinity and non-exhausted CD8 T cells against tumor self-antigens, does anti-RANKL enable ICB to reject poorly immunogenic tumors that would otherwise not respond? Using mouse tumors with naturally poor neoantigens or with depletion of strong neoantigens due to ICB relapse, we show that anti-RANKL potently restores ICB efficacy. Moreover, although blocking central tolerance with anti-RANKL might raise concerns for serious autoimmunity, surviving mice go on to live normal lifespans.
Thus, methods that interfere with central tolerance, like anti-RANKL, might help overcome a major limitation with ICB, which predominantly interferes with peripheral tolerance. This limitation, a T cell repertoire largely devoid of high-affinity TCRs against tumor antigens, may contribute to T cell exhaustion.
Transiently interfering with central tolerance generates a T cell repertoire that improves ICB against otherwise resistant tumors with depletion of strong neoantigens.
Interested in reading more?
Visit our publications page to see the pre-print!
Dhuey et al., bioRxiv, 2022.
Here Are Some of the People That Led The Studies and Made It Happen!
Erica Dhuey, grad student
Olivia Oldridge, former research specialist